Polycythemia Vera (PV)
The chronic blood condition polycythemia vera, sometimes known as PV, is a very uncommon but significant chronic blood disorder. A class of diseases known as myeloproliferative (MPNs), Polycythemia falls under this group. It is characterized by an excessive synthesis of different blood group types. White blood cells, red blood cells, and platelet production occur as PV, which primarily affects bone marrow. Polycythemia vera can have serious consequences if neglected., though it is not commonly seen as a type of cancer. Let's delve into the complexities of PV in this extensive guide, looking at its causes, symptoms, diagnosis, available treatments, potential side effects, and the significance of early discovery and management.
A) The Underlying Mechanisms of Polycythemia Vera
1)Pathophysiology of PV-A genetic mutation in the JAK2 gene, specifically the JAK2V617F mutation, has been linked to the onset of PV. The usual signaling pathways that control the bone marrow's ability to produce blood cells are interfered with by this mutation. Cells in the bone marrow therefore start to proliferate and increase uncontrollably, which causes an excess of blood cells, including platelets, white blood cells, and red blood cells.
2)Impact on Blood Composition Blood's composition significantly changes as a result of this aberrant cell growth. Notably, the quantity of red blood cells increases excessively, which can raise the hematocrit level (the proportion of red blood cells in the blood) considerably over normal levels. This affects the blood's viscosity and thickening
B) Symptoms of Polycythemia Vera
3)Pruritus (Itchy Skin): PV patients may experience itching, especially after a hot bath or shower, as a result of elevated histamine levels brought on by elevated white blood cell counts. PV sufferers may have painful and bothersome itchy skin.
4)Splenomegaly (Enlarged Spleen): PV can cause the spleen, an important organ situated in the upper left abdomen, to enlarge. In the affected location, an enlarged spleen may produce discomfort or even agony. The organ's function as a filter and regulator of blood cells causes this expansion, which is a reaction to the increasing production of blood cells.
5)Easy Bruising and Bleeding: PV's excessive platelet synthesis can interfere with the body's natural clotting and bleeding mechanisms. As a result, there may be a tendency for quick bruising and bleeding even on minor cuts.
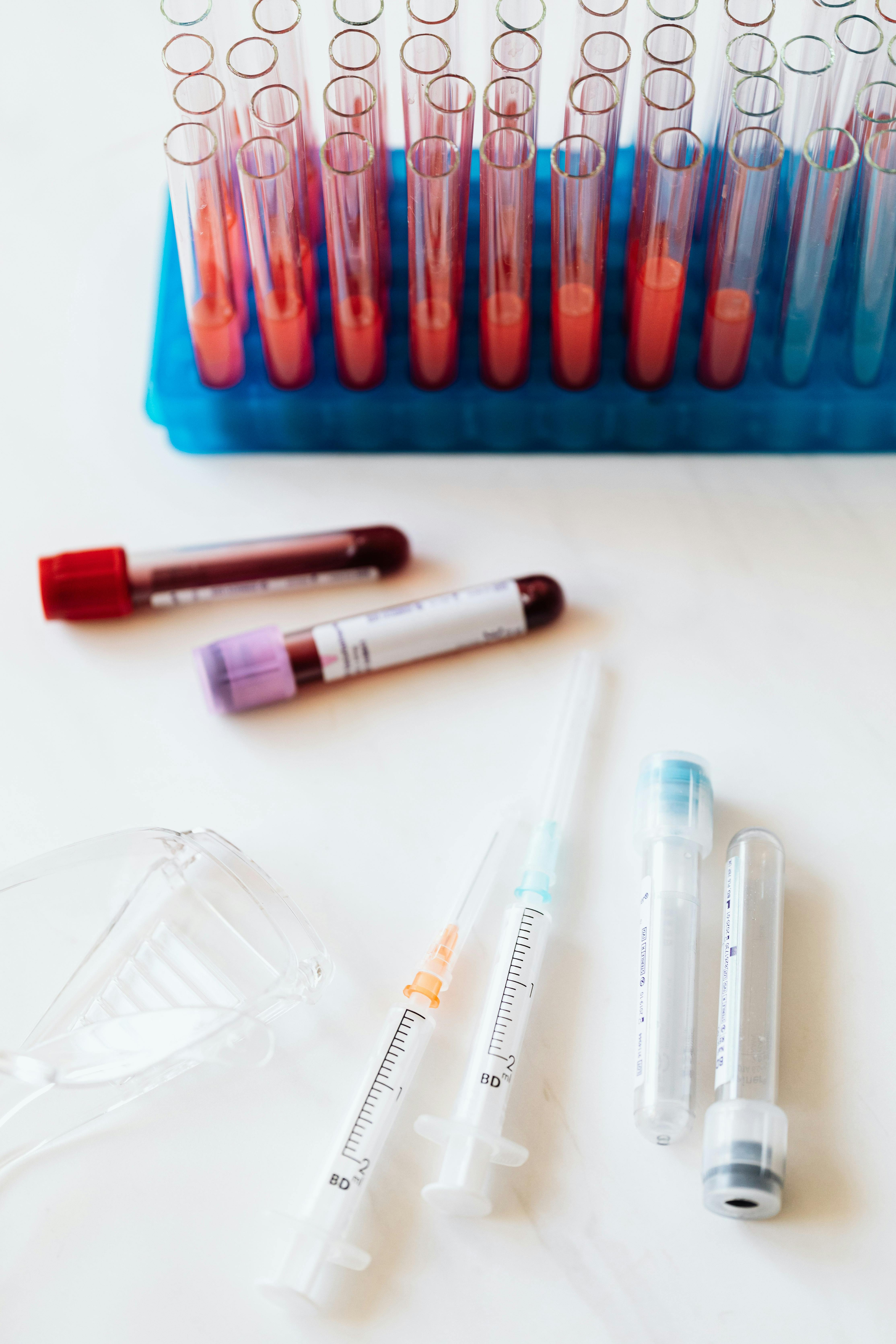
C)Diagnosis of Polycythemia
A number of medical examinations, including blood tests and, occasionally, a bone marrow biopsy, are necessary to diagnose PV. For determining the severity of PV and establishing its presence, several diagnostic procedures are crucial.
a-Complete Blood Count (CBC): A complete blood count is a common blood test that measures the quantities of different blood cells, such as platelets, white blood cells, and red blood cells. This test frequently indicates higher levels of these blood cells in PV patients. b-JAK2 Mutation Test: Determining if the JAK2V617F mutation is present is a critical diagnostic step. The majority of people with PV have this mutation, which is a crucial sign of the illness. c-Bone Marrow Biopsy: In some circumstances.
D)Treatment Options: Even though PV is a chronic illness, the correct treatment strategy can effectively manage it. Controlling the overproduction of blood cells, symptom relief, lowering the risk of complications, and enhancing the general quality of life are the main targets of treatment. Depending on the patient's age, general health, and PV severity, different treatments may be appropriate.
1)Phlebotomy: Bloodletting, often known as phlebotomy, is a frequent PV therapy strategy. It entails taking a certain volume of blood out of the body, usually through an arm vein. By lowering the hematocrit, this treatment also lowers blood viscosity. Phlebotomy treatments may be required on a regular basis to keep the right blood parameters.
2)Medications: Several drugs are used to treat PV and associated symptoms, including:
3)Hydroxyurea: A cytoreductive medication, hydroxyurea can assist in regulating the bone marrow's ability to produce blood cells. It is frequently recommended to increase blood flow and lower the risk of thrombosis.4)Ruxolitinib: Another medicine used to treat PV is roxolitinib. People who do not respond well to or cannot tolerate hydroxyurea will benefit the most from it.
6)Regular Check-Ups and Monitoring: PV management requires ongoing monitoring. Blood tests and regular check-ups are used to monitor the condition's development and alter treatment as necessary. These evaluations assist medical professionals in ensuring that the patient's blood parameters are within a safe range and that the medication is still working.
Water intake: Maintaining adequate water intake is crucial to fight the elevated blood viscosity linked to PV. Maintaining blood flow and lowering the chance of clot formation are both benefits of adequate hydration.
Diet: A healthy diet that is balanced and full of fruits, vegetables, and whole grains helps promote overall well-being. Some PV patients may need to restrict their intake of iron-rich foods since their frequent phlebotomy treatments can cause excessive iron absorption.
G) Support and Resources for Individuals with Polycythemia Vera
Healthcare Providers: It's critical to have a solid collaboration with healthcare providers. With your medical team, open lines of communication on a regular basis can help you address problems, modify treatment schedules, and guarantee the best care possible.
Support Groups: Becoming a member of a support group for people with PV can give them a sense of belonging and a place to discuss their experiences and coping mechanisms.
Educational Resources: There are many books, websites, and other educational resources available to assist people in better understanding PV and making decisions regarding their health.




No comments:
Post a Comment